What is Contrast-Enhanced Mammography (CEM)?
Contrast-enhanced mammography, also known as contrast-enhanced spectral mammography (CESM), is an advanced x-ray imaging technique that combines a standard mammogram with the injection of an iodine-based contrast agent. The contrast material highlights areas of increased blood flow, which is often associated with malignant tumors due to their ability to stimulate the growth of new blood vessels (angiogenesis).
How CEM Works
-
The patient receives an intravenous injection of an iodine-based contrast agent, typically a few minutes before the mammogram.
-
A dedicated CEM machine acquires two images of each breast – a low-energy image similar to a standard mammogram and a high-energy image that captures the contrast uptake.
-
The two images are then processed using sophisticated software to create a subtracted image that enhances areas of contrast uptake while suppressing background breast tissue.
-
The radiologist reviews the standard low-energy images, the contrast-enhanced images, and the subtracted images to identify any suspicious areas or abnormalities.
Advantages of CEM
-
Improved cancer detection: CEM has been shown to have higher sensitivity for detecting breast cancer compared to standard mammography, particularly in women with dense breast tissue.
-
Functional information: By highlighting areas of increased blood flow, CEM provides functional information about the breast tissue that can help differentiate between benign and malignant lesions.
-
Reduced recall rates: CEM may help reduce the number of false-positive results and unnecessary recalls for additional imaging or biopsies.
-
Faster and more accessible: CEM can be performed using existing mammography equipment with minor modifications, making it more accessible and cost-effective than breast MRI.
Limitations of CEM
-
Radiation exposure: CEM involves a slightly higher radiation dose compared to standard mammography due to the acquisition of two images per view.
-
Contrast risks: The use of iodine-based contrast agents carries a small risk of allergic reactions and potential complications in patients with impaired kidney function.
-
Limited availability: CEM is not yet widely available and may not be offered at all imaging centers.
What is Digital Breast Tomosynthesis (3D Mammography)?
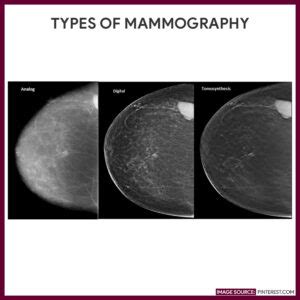
Digital breast tomosynthesis, commonly referred to as 3D mammography or DBT, is an advanced x-ray imaging technique that captures multiple low-dose images of the breast from different angles. These images are then reconstructed into a three-dimensional dataset, allowing radiologists to scroll through thin slices of the breast tissue and better visualize overlapping structures.
How 3D Mammography Works
-
The patient’s breast is positioned and compressed in a similar manner to a standard mammogram.
-
The x-ray tube moves in an arc over the breast, capturing multiple low-dose images from different angles.
-
The images are then reconstructed using advanced computer algorithms to create a 3D dataset of the breast tissue.
-
The radiologist can scroll through the thin slices of the breast tissue in the 3D dataset, minimizing the impact of overlapping structures and improving lesion visibility.
Advantages of 3D Mammography
-
Improved cancer detection: Studies have shown that 3D mammography can detect more cancers than standard 2D mammography, particularly in women with dense breast tissue.
-
Reduced recall rates: By minimizing the impact of overlapping structures, 3D mammography can help reduce false-positive results and the need for additional imaging or biopsies.
-
Better lesion characterization: The ability to scroll through thin slices of breast tissue allows radiologists to better characterize the size, shape, and location of suspicious lesions.
-
Increased patient comfort: Some women report less discomfort during 3D mammography due to the reduced need for additional compression views.
Limitations of 3D Mammography
-
Increased reading time: Interpreting 3D mammography studies takes longer than standard 2D mammograms due to the larger number of images to review.
-
Higher radiation dose: Early 3D mammography systems involved a higher radiation dose compared to standard mammography. However, newer systems have been developed that reduce the radiation dose to levels comparable to or even lower than standard mammography.
-
Cost and availability: 3D mammography equipment is more expensive than standard mammography machines, and not all imaging centers may offer this technology.
CEM vs. 3D Mammogram: Key Differences
| Feature | CEM | 3D Mammogram |
|---|---|---|
| Imaging Technique | Combines standard mammogram with iodine-based contrast injection | Captures multiple low-dose images from different angles to create a 3D dataset |
| Information Provided | Functional information (blood flow) | Structural information (breast tissue architecture) |
| Cancer Detection | Higher sensitivity, particularly in dense breasts | Improved detection, particularly in dense breasts |
| Recall Rates | May reduce false-positives and unnecessary recalls | Reduces false-positives and unnecessary recalls |
| Radiation Dose | Slightly higher than standard mammography | Comparable to or lower than standard mammography with newer systems |
| Contrast Risks | Small risk of allergic reactions and kidney complications | No contrast risks |
| Availability | Limited, not widely available | Increasingly available, but not offered at all centers |
| Cost | More accessible and cost-effective than breast MRI | More expensive than standard mammography equipment |

Frequently Asked Questions (FAQ)
-
Who should consider getting a CEM or 3D mammogram?
Women with dense breast tissue, a personal history of breast cancer, or a strong family history of the disease may benefit from CEM or 3D mammography. However, the decision to undergo these advanced imaging techniques should be made in consultation with a healthcare provider, taking into account individual risk factors and screening guidelines. -
Are CEM and 3D mammography covered by insurance?
Coverage for CEM and 3D mammography varies by insurance provider and plan. Many insurance companies now cover 3D mammography as part of their standard breast cancer screening benefits. CEM coverage may be more limited, and patients should check with their insurance provider to determine their specific coverage and any out-of-pocket costs. -
How often should I get a CEM or 3D mammogram?
The frequency of CEM or 3D mammography screening depends on individual risk factors and screening guidelines. In general, women at average risk for breast cancer are recommended to have annual mammograms starting at age 40 or 50, depending on the specific guidelines followed. Women at higher risk may benefit from earlier or more frequent screening. It is essential to discuss your individual screening plan with your healthcare provider. -
Are there any risks associated with CEM or 3D mammography?
Both CEM and 3D mammography involve exposure to ionizing radiation, which carries a small potential risk. However, the radiation dose used in these techniques is considered low, and the benefits of early cancer detection generally outweigh the risks. CEM also involves the use of iodine-based contrast agents, which can cause allergic reactions in some patients and may not be suitable for those with impaired kidney function. -
Can CEM or 3D mammography replace other breast imaging techniques, such as ultrasound or MRI?
While CEM and 3D mammography are powerful tools for detecting breast cancer, they do not replace other imaging modalities in all cases. Ultrasound and MRI may still be recommended for further evaluation of suspicious findings or for screening high-risk patients. Each imaging technique has its strengths and limitations, and the choice of modality depends on the individual patient’s needs and circumstances.
Conclusion
Contrast-enhanced mammography (CEM) and digital breast tomosynthesis (3D mammography) are advanced breast imaging techniques that aim to improve the early detection of breast cancer. While both modalities offer advantages over standard 2D mammography, they differ in their imaging approach, the information they provide, and their specific benefits and limitations.
CEM combines a standard mammogram with the injection of an iodine-based contrast agent to highlight areas of increased blood flow, providing functional information that can help differentiate between benign and malignant lesions. 3D mammography, on the other hand, captures multiple low-dose images of the breast from different angles to create a three-dimensional dataset, allowing for better visualization of overlapping structures and improved lesion characterization.
Both CEM and 3D mammography have been shown to improve cancer detection rates, particularly in women with dense breast tissue, and may help reduce false-positive results and unnecessary recalls. However, they also have some limitations, such as slightly higher radiation doses (for CEM and older 3D mammography systems), contrast risks (for CEM), and limited availability and higher costs compared to standard mammography.
Ultimately, the choice between CEM and 3D mammography depends on individual patient factors, available resources, and the expertise of the imaging center and radiologists. As these technologies continue to evolve and become more widely available, they have the potential to significantly improve breast cancer screening and early detection, leading to better outcomes for patients.
No responses yet